The Detrimental Interplay of COVID-19 with Diabetes
Anindro Bhattacharya, Hareem Bilal (edited by Annam Imran)
Posted on 28 Feb, 2021
Introduction
It seems almost an understatement to claim that millions of people around the world have been impacted by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)--the virus behind the COVID-19 pandemic. As of April 2021, there have been around 132 million confirmed cases of COVID-19 and 2.9 million deaths reported to the World Health Organization (World Health Organization 2021). WHO declared the COVID-19 outbreak a public health emergency. In particular, the organization warned individuals with pre-existing medical conditions, such as diabetes, to be extra vigilant due to the virus’ disproportionate impacts on these populations (Assaloni et. al 2020). Unfortunately, people living with diabetes are 2.85 times more likely to die from COVID-19 than non-diabetic patients (Diabetes Canada 2021). The biological implications of the virus, as well as the drastic changes in living due to worldwide lockdowns, has negatively affected diabetic patients both physically and mentally (Ghosh et. al 2020).
COVID-19’s interference with the body’s regulatory processes
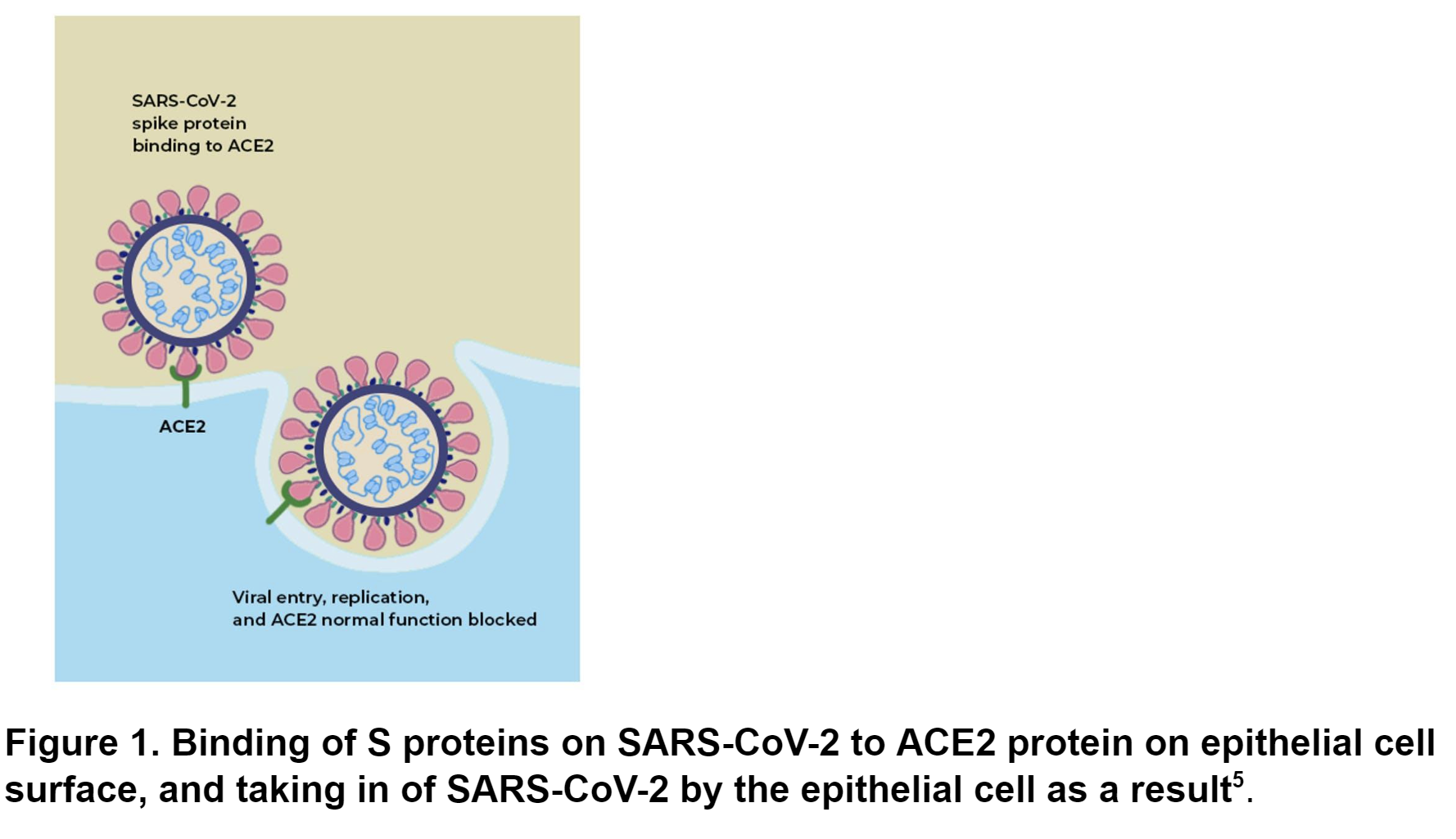
Diabetes is a disease characterized by the body’s inability to produce insulin or sufficiently use the insulin that it produces. Insulin is a molecule produced by the pancreas (an organ in the digestive system) that regulates the amount of sugar in the blood; too much sugar in the blood damages organs, blood vessels, and nerves, restricting the body from receiving enough energy. Through COVID-19’s interference in the body’s regulatory processes, diabetic patients are unfortunately placed at a greater risk of morbidity (or risk for contracting COVID-19 (Diabetes Canada 2021). COVID-19, which is a respiratory disease, enters the body through the airway. Once in the body, the surface proteins on the virus, called spike (S) proteins, bind specifically to a type of protein, angiotensin-converting enzyme-II (ACE2), found on the surface of epithelial cells (such as cells in the blood vessels or the lining of organs). This binding of S to ACE2 signals the epithelial cell to engulf the virus and ACE2 becomes ineffective after being brought inside the cell (Sriram etl. al 2021) (Fig. 1).
Along with other functions, ACE2 is primarily known to be involved in a system that maintains blood pressure (which is the pressure of blood exerted on the walls of blood vessels). ACE2 promotes the expansion of blood vessels, which lowers blood pressure (Clutter 2020). However, high blood pressure is very common in diabetic patients as sugar remains in the bloodstream due to the body’s inability to metabolize (or use) sugar instead of allowing the sugar to enter cells and be converted to energy. The high concentration of sugar in the cells, therefore, contributes to high blood pressure by increasing the amount of chemicals carried in the blood that will hit the blood vessel walls (Schofield et. al 2020). With COVID-19 rendering ACE2 inactive (as demonstrated in Fig. 1), the body is not able to lower high blood pressure, which may lead to fatal consequences such as heart attack or stroke. Another possible complication of high blood pressure over an extended period of time is diabetic nephropathy, a condition in which the high pressure of the blood damages the delicate blood vessels found in the kidney. This damage can be irreversible and may require dialysis or a kidney transplant for survival (Mayo Clinic 2021). ACE2 also helps promote optimal beta cell function. Beta cells are a type of cell in the pancreas which secretes insulin to decrease blood sugar levels. To begin with, insulin insufficiently regulates blood levels in diabetic patients. When ACE2 is blocked by COVID-19, insulin’s regulation of blood sugar is further reduced, resulting in greater inability of the body to independently control the blood sugar (Schofield et. al 2020). Overall, COVID-19 jeopardizes the regulatory functions in the body that help maintain blood pressure, resulting in a compounding effect on diabetic patients, which can lead to serious complications.
The Impact of COVID-19 on Diet and Physical Activity
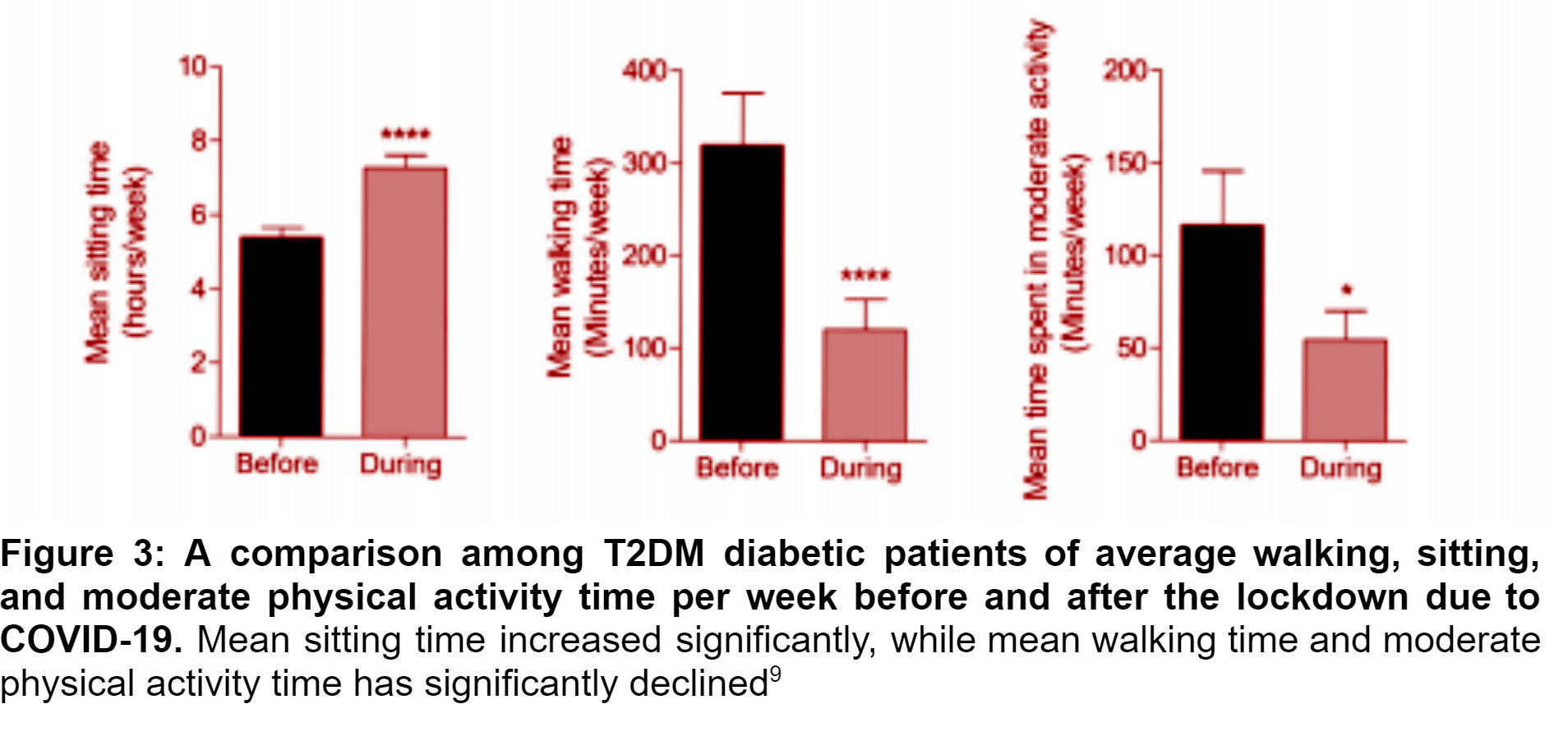
The indirect impacts of the COVID-19 pandemic also contribute to the increased mortality (or death rate) of diabetic patients. Diet and physical activity help manage diabetes, and any major disruption of healthy lifestyle routines can become a health risk for diabetic patients (Ruiz-Roso et. al 2020). This is especially true for type 2 diabetic patients (T2DM), which are individuals with a type of diabetes often caused by lifestyle choices and diet. Health organizations such as WHO and the Spanish Academy of Nutrition and Diabetes attest to the importance of diet and physical activity as factors that will help manage diseases like diabetes. The COVID-19 pandemic has decreased access to healthcare as patients are advised to stay home unless severely ill. As a consequence, T2DM patients have faced difficulty managing their condition, which is made worse by the fact that virtual consultations have become largely the sole option of gaining medical advice (Ruiz-Roso et. al 2020). A study conducted in North India showed that throughout the pandemic and quarantine, consumption of sugary foods by T2DM patients increased by 21%, snacking increased by 23%, but physical activity declined by 42%; 19% of T2DM patients gained weight. These behaviours promote the weight gain observed among patients with T2DM (Ghosh et. al 2020). Rapid gain in weight leads to obesity, resulting in increased mortality in T2DM patients (Ross et. al 2011). Another study conducted at the University of Hospital La Princesa (Madrid, Spain) examined the impact of the lockdown on nutrition, physical activity and psychological health of T2DM patients (Ruiz-Roso et. al 2020). The inclusion criteria for the study was male or female adults, aged 40 to 80, who were previously diagnosed with T2DM, with body mass indexes (BMI) ranging from 25kg/m2 to 40 kg/m2, which fall within the overweight range. A total of 72 patients with an average age of 63 participated, where 48% were male and 51% were female. A significantly increased intake of “junk food” was most notable compared to more nutritious foods, such as vegetables (Fig. 2). Among the participants, 74.3% did not consume sugary foods before the lockdown, but this number decreased to 67.1% during the lockdown (Ruiz-Roso et. al 2020). Unhealthy intake of sugar results in poor ability to maintain healthy levels of sugar in the blood, which can be detrimental for diabetic patients, as healthy blood sugar levels prevent organ damage and other complications caused by diabetes (Haghighatpanah et. al 2018). There was an observed decline in the average weekly time spent doing physical activity by T2DM patients (Fig. 3). Numerous studies have indicated that physically active individuals have a lower risk of developing T2DM (Ruiz-Roso et. al 2020). Physical activity can aid in lowering levels of obesity, which in turn can prevent T2DM in healthy individuals (Kirwan et. al 2017).
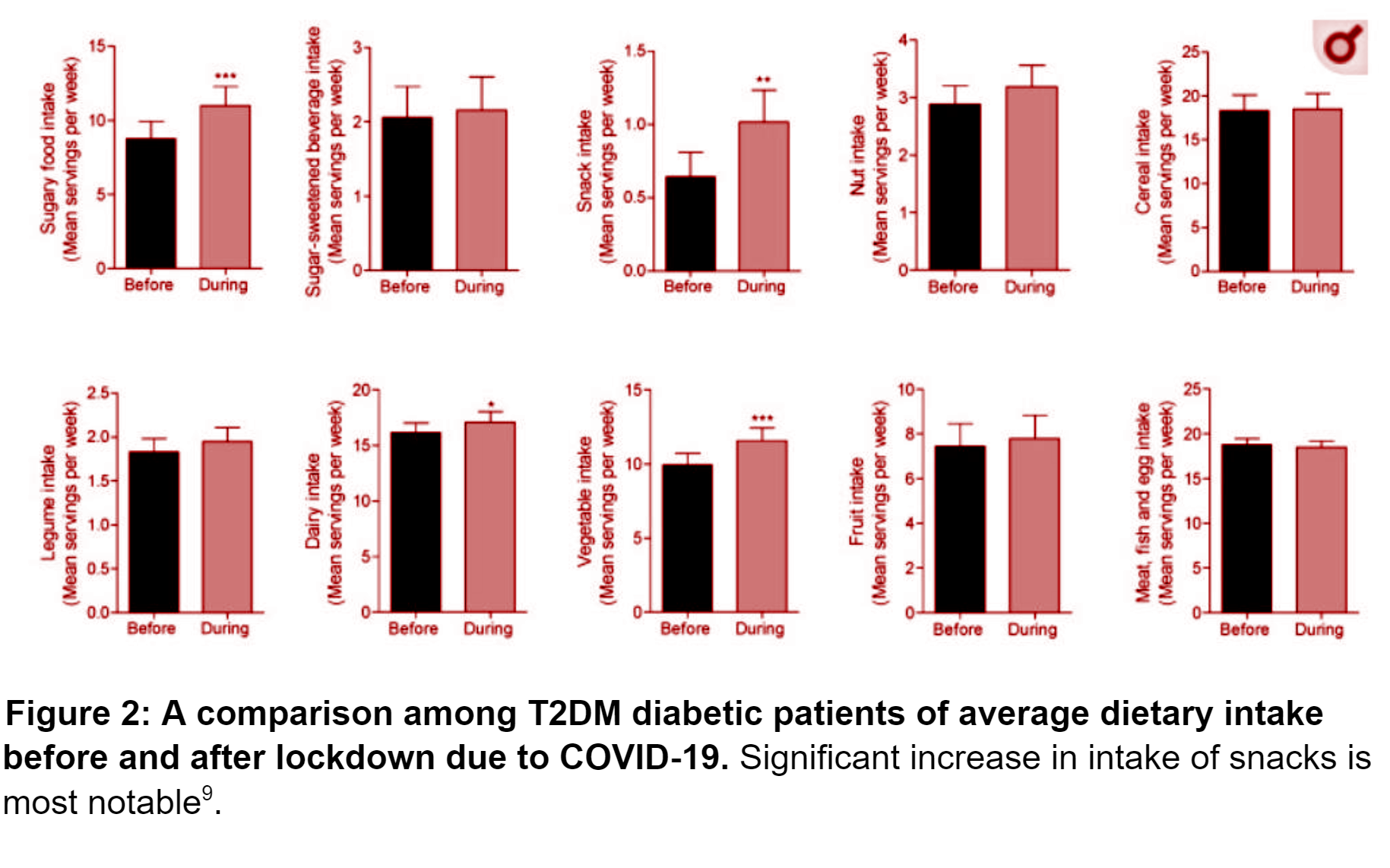
Ruiz-Roso et al. (2020) strongly emphasizes the significance of its findings and supports the need for health policies that promote a healthy lifestyle during the pandemic, especially when it comes to physical activity and dietary habits. A thorough analysis and research on the patterns in physical activity and diet will help national health authorities prepare and aid patients with T2DM, for this pandemic and for future global lockdowns, disasters, and pandemics.
Conclusion
The biological interactions between the virus and the body’s regulatory mechanisms alongside the sheer change in lifestyle as a result of the pandemic have had a compounded impact on the overall health of diabetic patients. SARS-CoV-2 targets the ACE-2 enzyme, which is involved in biological pathways responsible for regulating blood pressure and blood sugar in the body. Jeopardizing the functions of this integral enzyme places diabetic patients at risk for further complications, such as heart attack or stroke. Additionally, lockdown measures have resulted in a shift to a more sedentary lifestyle among the greater population due to restricted access to gyms and parks. These drastic changes have left diabetic patients more vulnerable during the pandemic. According to Riddle et al. (2020), among the initial patients diagnosed with COVID-19 in China in early 2020, the mortality rate of patients with pre-existing diabetes was 7.3%, which is three times more than that of the overall population.. A second Chinese report on hospitalized patients found that 19% were previously diagnosed with diabetes (Riddle et. al 2020). In 2019, the prevalence of diabetes globally was estimated to be 9.3% (463 million people) and is predicted to rise to 10.2% (578 million people) in 2030 (Saeedi et. al 2019). Although diabetic patients might face worse complications if diagnosed with COVID-19, there is not enough data present that indicates whether diabetic patients are more susceptible to the virus (American Diabetes Association 2021). Perhaps through awareness programs organized by local public health agencies as well as check-ups with their general physicians, diabetic patients could be educated about how they can modify their diet and lifestyle to reduce the risk of succumbing to the unfortunate repercussions of the virus.
Glossary:
- ACE2: angiotensin-converting enzyme-II; protein found in various organs around the body, including the lungs, heart, kidney, intestines, liver and brain which helps expand blood vessels to reduce blood pressure
- Beta cells: type of cell in the pancreas which secrete insulin to decrease blood sugar levels
- Blood pressure: pressure of blood exerted on the walls of blood vessels, which increases with the amount of chemicals and molecules in the blood
- BMI: Body Mass Index (BMI) is a person's weight in kilograms divided by the square of height in meters. A high BMI can be an indicator of high body fatness
- Diabetic nephropathy: a condition in which the high pressure of the blood damages the delicate blood vessels found in the kidney
- Dialysis: treatment in which an external machine filters waste out of the blood
- Epithelial cells: cells that line cover any of the body’s surfaces, including hollow organs
- Insulin: a molecule produced by the pancreas (accessory organ in the digestive system) that regulates the amount of sugar in the blood; too much sugar in the blood for long periods of time can lead to heart diseases and complications; too little sugar in the blood leads to dizziness and low energy
- Metabolize: the biological process through which food can be chemically changed into form that can be used by the body
- Morbidity: the amount of a specific disease in a population
- Mortality: a term used for death rate, or the number of deaths in a certain group of people in a certain period of time.
- Spike protein (S): surface proteins on the coronavirus
- T2DM: classification of diabetes in which the body does not produce enough insulin
References:
WHO Coronavirus (COVID-19) Dashboard. World Health Organization. [accessed 2021 Apr 8]. https://covid19.who.int/
Assaloni R, Pellino VC, Puci MV, Ferraro OE, Lovecchio N, Girelli A, Vandoni M. Coronavirus disease (Covid-19): How does the exercise practice in active people with type 1 diabetes change? A preliminary survey. Diabetes research and clinical practice. 2020;166(108297):108297.
What is diabetes? Diabetes Canada. [accessed 2021 Jan 7]. https://www.diabetes.ca/about-diabetes/what-is-diabetes
Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes & metabolic syndrome. 2020;14(5):917–920.
Sriram K, Insel P, Loomba R. 2020 May 14. What is the ACE2 receptor, how is it connected to coronavirus and why might it be key to treating COVID-19? The experts explain. The Conversation. [accessed 2021 Jan 7]. http://theconversation.com/what-is-the-ace2-receptor-how-is-it-connected-to-coronavirus-and-why-might-it-be-key-to-treating-covid-19-the-experts-explain-136928.
Clutter C. The Biology and Immunology of COVID-19 Susceptibility. American Society for Microbiology. 2020 Jun 5 [accessed 2021 Jan 7]. https://asm.org/Articles/2020/June/The-Biology-and-Immunology-of-COVID-19-Susceptibil
Schofield J, Leelarathna L, Thabit H. 2020. COVID-19: Impact of and on diabetes. Diabetes Ther. 11(7):1429–1435.
Diabetic nephropathy. Mayo Clinic. [accessed 2021 Feb 27]. https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/symptoms-causes/syc-20354556
Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, Marazuela M. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with Type 2 Diabetes Mellitus. Nutrients. 2020;12(8):2327.
Ross SA, Dzida G, Vora J, Khunti K, Kaiser M, Ligthelm RJ. Impact of weight gain on outcomes in type 2 diabetes. Current medical research and opinion. 2011;27(7):1431–1438.
Haghighatpanah M, Nejad ASM, Haghighatpanah M, Thunga G, Mallayasamy S. 2018. Factors that correlate with poor glycemic control in Type 2 Diabetes Mellitus patients with complications. Osong Public Health Res Perspect. 9(4):167-174. Available from: https://doi.org/10.24174/j.phrp.2018.9.4.05.
Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleveland Clinic journal of medicine. 2017;84(7 Suppl 1):S15–S21.
Riddle MC, Buse JB, Franks PW, Knowler WC, Ratner RE, Selvin E, Wexler DJ, Kahn SE. COVID-19 in people with diabetes: Urgently needed lessons from early reports. Diabetes care. 2020;43(7):1378–1381.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes research and clinical practice. 2019;157(107843):107843.
Frequently asked questions: COVID-19 and diabetes. American Diabetes Association. [accessed 2021 Feb 27]. https://www.diabetes.org/coronavirus-covid-19/how-coronavirus-impacts-people-with-diabetes